SOAP A chart note usually follows a very simple pattern Subjective (what the patient thinks) = S Objective (what the doctor thinks) = O Assessment (what the diagnosis is) = A Plan (what happens next) = P Not all providers dictate the "SOAP" note format;List of 3 best SOAP meaning forms based on popularity Most common SOAP abbreviation full forms updated in July 21Taken from Massage Therapy, Principles and Practice, 3rd edition by Susan Salvo Learn with flashcards, games, and more — for free
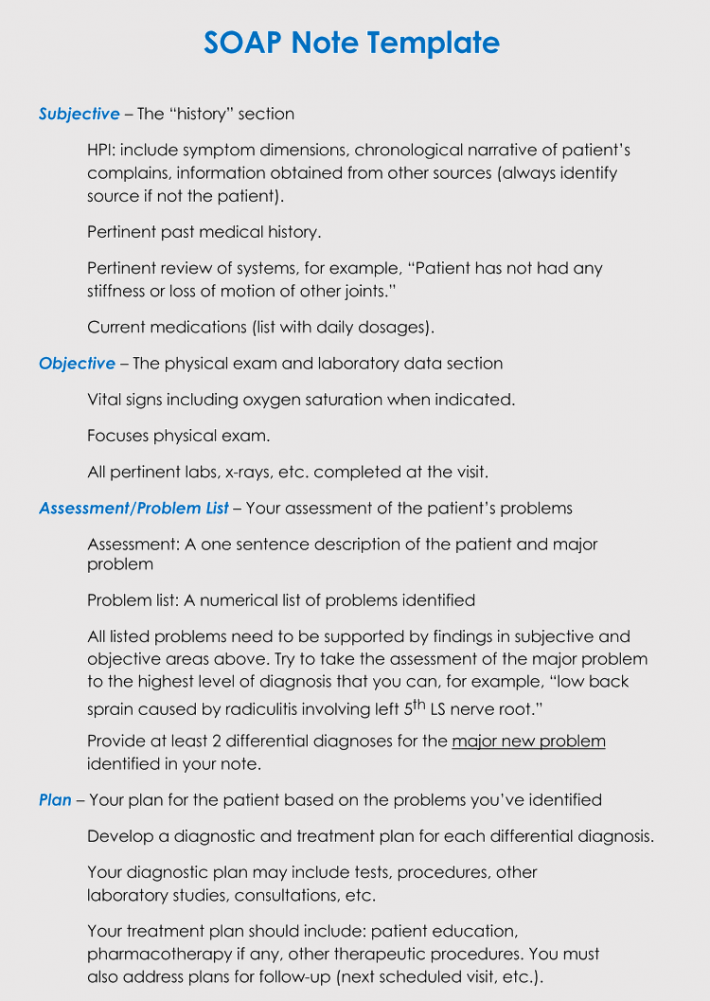
30 Soap Note Examples Blank Formats Templates
